Asia Pacific Journal of Family Medicine Volume 5 Issue 2
VIEWPOINT
Rethinking general practice – Part 1: Far from equilibrium disease-centred and
econometric-oriented health care and general practice/family medicine
Joachim P. STURMBERG1 and Carmel M. MARTIN2

Accepted for publication 27 March 2006.
Rethinking general practice – Part 1: Far from equilibrium disease-centred and
econometric-oriented health care and general practice/family medicine
Joachim P. STURMBERG1 and Carmel M. MARTIN2
1Department of General Practice, Monash University, Melbourne, Victoria, Australia and 2Clinical Sciences, Northern Ontario School of Medicine, Sudbury, Canada
Correspondence: Associate Professor Joachim Sturmberg, PO Box 3010 , Wamberal, New South Wales , 2260, Australia.Accepted for publication 27 March 2006.
Abstract
Background: Internationally, health care systems are struggling in an increasingly costly medical environment to satisfy population needs and demands. Narrow understandings of ‘health’ and ‘budgets’ dominate health system management and drive the reforms needed to adapt to the new challenges. Caught up in this unsustainable environment the general practitioner/family physician is challenged to operate effectively, while having lost his/her role definition.
Objectives: This paper is the first of a two-part series. In this paper we argue that health needs to be understood in broad terms. A complex systems framework is used to integrate the diverse needs within the health care system that sits under the umbrella of a social understanding of health. We argue that this allows for a better understanding of the challenges of a socially complex patient-focused general practice role in the health system. In the second paper in this two-part series we suggest ways forward toward a patient/illness-centred health system
Key issues: The complexities of a ‘health care system’ are explained using a vortex model with the patient and his/her health at the centre. The somato-psycho-socio-semiotic paradigm assists the understanding of primary health care (PHC) as a multifaceted system constructed around patient and community care with the clinical encounter at its centre. Patients and their communities are linked in a multidimensional ‘health system’. This includes other entities such as education, welfare, social justice systems, in addition to financial and tertiary-care type measurable disease features that traditionally define ‘health care effectiveness and efficiency’ This model depicts non-linear dynamic interdependencies and accountabilities within and among policies, the local environment, the clinical encounter and their cellular consequences. Practicing and teaching ‘patient-centred’ general practice care involves recognition of the social connectedness of the key actors – individual patients plus their practitioners, and the self-organizing capacity inherent in much of health care. The health system though is an interconnected, multilevelled, highly contextualized, dynamically adaptive social organization. During this period of continual reforms the role confusion experienced in general practice can be addressed with a deeper understanding of the nature of health, illness and disease and the socio-economic climate, so that all levels of providers are ultimately able to discharge their accountability to patients, communities and the population.
Conclusion: In spite of the diverse range of challenges, general practice must promote a ‘change vision’ using a strategy that integrates and focuses on front-line providers. This has to meet patients’ individual needs at the point of care, despite economic and tertiary care disease model drivers. General practice is ultimately accountable to the patient, the community and the population to improve their health experiences with a realignment to a broader vision of health care.
Key words: complexity, general practice, health systems, knowledge management, leadership, primary health care
Objectives: This paper is the first of a two-part series. In this paper we argue that health needs to be understood in broad terms. A complex systems framework is used to integrate the diverse needs within the health care system that sits under the umbrella of a social understanding of health. We argue that this allows for a better understanding of the challenges of a socially complex patient-focused general practice role in the health system. In the second paper in this two-part series we suggest ways forward toward a patient/illness-centred health system
Key issues: The complexities of a ‘health care system’ are explained using a vortex model with the patient and his/her health at the centre. The somato-psycho-socio-semiotic paradigm assists the understanding of primary health care (PHC) as a multifaceted system constructed around patient and community care with the clinical encounter at its centre. Patients and their communities are linked in a multidimensional ‘health system’. This includes other entities such as education, welfare, social justice systems, in addition to financial and tertiary-care type measurable disease features that traditionally define ‘health care effectiveness and efficiency’ This model depicts non-linear dynamic interdependencies and accountabilities within and among policies, the local environment, the clinical encounter and their cellular consequences. Practicing and teaching ‘patient-centred’ general practice care involves recognition of the social connectedness of the key actors – individual patients plus their practitioners, and the self-organizing capacity inherent in much of health care. The health system though is an interconnected, multilevelled, highly contextualized, dynamically adaptive social organization. During this period of continual reforms the role confusion experienced in general practice can be addressed with a deeper understanding of the nature of health, illness and disease and the socio-economic climate, so that all levels of providers are ultimately able to discharge their accountability to patients, communities and the population.
Conclusion: In spite of the diverse range of challenges, general practice must promote a ‘change vision’ using a strategy that integrates and focuses on front-line providers. This has to meet patients’ individual needs at the point of care, despite economic and tertiary care disease model drivers. General practice is ultimately accountable to the patient, the community and the population to improve their health experiences with a realignment to a broader vision of health care.
Key words: complexity, general practice, health systems, knowledge management, leadership, primary health care
Subject matter … do not … constitute a basis for distinguishing disciplines. Disciplines are distinguished partly for historical reasons and reasons of administrative convenience … And partly because the theories that we construct to solve our problems have a tendency to grow into unified systems. But all this classification and distinction is a comparatively superficial affair. We are not students of some subject matter but students of problems. And problems may cut right across the borders of any subject matter or discipline. (K.Popper, 1972),1Health care systems in the developed world, including countries such as the US, Canada, the UK, Germany and Australia are barely coping with the varied demands placed on them. ‘Budgets’ rather than ‘health’ appear to drive politicians and bureaucrats in Health Departments on the one hand and medical and pharmaceutical corporations in the private sector on the other (Fig. 1). Measurable discrete changes in ‘health outcomes’ have become the currency in the competition for budget allocations. These – usually surrogate – measures are more readily obtainable within the acute care setting, hospital-based services and certain community and practice activities. These services have a financial advantage over other patterns of care.2 The consequences of such an approach have exposed structural and philosophical deficiencies inherent in a ‘disease industry’ driven system and reveal a limited understanding of the benefits inherent in primary health care. The logic is simple – every health event prevented is one that cannot be counted, hence it does not need any budget allocation.3
The complexities of health ‘care’
The complexities and competing interests in health care provision in the ‘health market place’ are demonstrated in such health system ‘tensions’ as:
• highly structured hospital care versus sophisticated and comprehensive community-based care;
• resource allocation to latest technology versus chronic care management;
• individual patient care versus public health care;
• comparison of access to health care for underserved communities and the ‘nice suburbs’;
• workforce supply between low and high socio-economic areas;
• corporatist ownership and managerial control versus responsible local management by health care providers; and
• emphasis on cure of organ systems versus care for people, and so forth.4
Definitions of health care
‘Health care’ can be simplified by narrowly focusing on what doctors and allied health workers provide when confronted with patient diseases, or patient demands. On the other hand, ‘health care’ can be broadly seen as the complex societal activities in which health professionals engage in the interests of well and sick people.
However, embracing the complexities inherent in ‘good health care’ requires both governments, industry and society at large, together with the health, education and welfare sectors to assess the impact of economic, employment, justice, education, health, environmental, capital works and other policies for their potential negative effect on our ‘health’ and ‘social capital’.
The patient in the centre of the health ‘care’ system
Our analysis is based on the fundamental assumption that the focus of any health care system should be governed by its patients’ needs. Hence we embrace the complexities associated with planning and providing ‘patient-centred health care’ services.
The comprehensive health care needs of individuals have been well described through the somato-psycho-socio-semiotic paradigm5 which is based on the observation that ‘healing’ the patient is not achieved by solely addressing the biological components of his disease. To achieve healing it is equally important to address the social and psychological aspects of the complaint, and most of all one has to help the patient to find meaning (semiotics: interpreting the signals of the disease) in his illness experience. As Per Fugelli put it so eloquently: ‘You cannot feel disease, you only can feel its consequences.’6
To fully appreciate the implications inherent in the somato-psycho-socio-semiotic paradigm of ‘health’ requires one’s thinking to shift toward a systems approach.7 The key characteristics of any system are its pattern, structure and processes, and the fact that despite the changes occurring within the system it is able to maintain itself.8 In short, within a system all its components are interconnected, hence a change in one component will affect all other components. Indeed it has been shown that understanding the connections between components of a system is more important than understanding the components themselves.9
Metaphorically the complexities of the ‘health care system’ can be compared to a vortex. All the elements making up the ‘health care system’ exert their pressure onto the ‘health’ of the individual’s cells through their effects on the person’s environment and their effects on the balance of his somato-psycho-socio-semiotic needs (Fig. 2). Minor changes to a single element within the system can have major, and often unforeseen, consequences on the whole system.
In the following section we describe how the disease-focused system maintains itself and how this affects primary care.
Dominance of the disease over the illness model
Currently the system does not place ‘health’ at the centre of all considerations. The dominance of the ‘disease’ over the ‘illness’ model will perpetuate its own ‘disease-focused stability’, supported by the current mode of medical practice and teaching (Fig. 3).
Medical practice
Consultations invariably occur within a disease-focused framework – most of the time the patient’s story is interrupted after only 18 seconds10 by closed questions that seek disease-specific information. However, understanding the patient’s story is the prerequisite to helping patients gain an understanding of their illness. Open questions and time are required, but time is seen by the system as too expensive a resource (see below). Quickly ordering an investigation or prescribing a drug is the way to constrain consultation length.11
Not surprisingly large numbers of patients are referred to specialists, even though approximately half do not have a specific disease.12,13 This may reassure the referring doctor; however, no disease being found is often not reassuring for the patient, who still needs ‘an answer’ to ‘the illness experience’. Medicine’s preoccupation with ‘cure of the disease’ has become counterproductive; ‘care for the illness’ is needed – through its psycho-neuro-immunological properties, caring achieves improved ‘health’ and ‘measurable health outcomes/health status’.14
The disease approach largely ignores the forces exerted by the top of the vortex, that is, the context of the patient and societal structures, and uses as its starting point the cellular level. The illness approach, that is, the engagement with the patient recognizes the importance of cellular knowledge, but actively involves the knowledge exerted by the elements at the top of the vortex.
Medical education
‘Experts’ in the ‘diseases’ provide most of the medical education in universities and teaching hospitals. Their practice patterns are invariably limited to a narrow patient range (also known as selection bias); therefore it is not surprising that their teaching focuses on pathologies, disease manifestations, investigations and treatments of the organ-systems they are familiar with. This approach to teaching reinforces medicine’s fragmentation and specialization.15
Medical curricula have not changed in spite of evidence that firstly, most disease occurs in the community16 and secondly, 40–50% of all patients referred to specialist outpatient services have no organic disease found.12,13 Overall little attention is given to the study of the ‘sciences of illness’, that is, the context in which THIS patient’s illness occurs, issues of quality of life of the patient and his family, and the integration of the wider societal aspects on the patient’s life.
Hence it is no surprise that large amounts of resources are wasted in unnecessary procedures while somatization as a cause of physical symptoms is largely ignored.17 In recent years the legal profession helped to perpetuate the disease emphasis by only accepting ‘hard data’, rather than clinical reasoning, as defensible evidence.
Unsustainability of the disease over the illness model
There is clear evidence that the prevailing disease-focus within the health system is not sustainable. Four rather disparate issues put pressure on the system and will force changes to be made:
• medical progress through rapidly developing technologies;
• degradation of social structures through rising socio-economic disparities;
• the economic rationalist paradigm through a shift away from health outcomes; and
• changing health policy priorities through changing demographics and the pressures exerted by the other three issues (Fig. 4).
Medical progress
Technological advances, above all, have enabled the medical profession to diagnose many more cases of any given disease at a very early stage. This has fostered an apparent increase in prevalence of most diseases without an obvious decrease in their respective absolute mortality.18–21 However, very little is known about the natural history of early disease, and even less is known about the benefit of treating ‘incidental’ findings in otherwise perfectly healthy people. These developments exert pressure on the health care system in two ways – first, there is an increased demand for more specialist doctors to deal with these ‘diseases’, and second, since these doctors usually cannot do anything much about these problems, patients are seen more frequently for simple surveillance, leading to a spiralling demand within the whole system.18
Degrading social structures
Two factors that greatly impact on health and wellbeing are socio-economic disparities and the loss of community and social capital. Recently there has been a rediscovery of large and persistent socioeconomic and racial-ethnic disparities in health. Socioeconomic position and race/ethnicity shape individuals’ exposure to and experience of virtually all known psychosocial, as well as many environmental and biomedical risk factors, and these risk factors help to explain the size and persistence of social disparities in health.22 Poverty is linked to poor health on an individual as well as a country level in both developing (absolute poverty) and developed countries (relative poverty). The reasons are complex with, on the one hand, poor health causing poor economic performance, and on the other, the maldistribution of resources across a society – especially the poor, which independently impacts on health and human development. Investing in public health is a prerequisite to reducing poverty and increasing economic output and living standards.23
Increasing economic inequality also decreases social cohesion, increases individual malaise, and produces the conditions by which increased mortality and morbidity occurs.24 The importance of social support in terms of reducing mortality and morbidity has been established.25 Social support is exerted through social networks, the quality of these relationships and the recourses they provide. Loss of social support is evidenced in measures like the rise of marital and family break-up, and the decline in participation of voluntary community institutions.
Economic pressures
Until recently, medical care was largely provided through a publicly supported policy and financing framework (except in the US). Emerging knowledge suggests that methods of health services funding influence the way providers practice medicine.26 Today there is a worldwide trend for ‘health care’ to be determined through an economic rationing paradigm. The most widely used approach is managed care, which refers to systems and techniques used to control the use of health care services. Mechanisms include:
• a review of medical necessity;
• incentives to use certain providers; and
• case management around a financially based plan.
Usually the drivers are directed toward managing financial risk and containing care to protocols and formulae.27
The fee-for-service system is popular among providers, simply because it gives them a sense of control over their enterprise. Many argue that all forms of physician remuneration will distort the effectiveness and efficiency of the health care system in some way. Even blended models, although theoretically able to address problems of all other remuneration types, may be complex to administer and have other unknown consequences. Over and above any unintended perverse incentives, the HMO system in the US has been accused of manipulating the provision of health care by coercive medical contracts and cooperative management structures that solely aim at maximizing shareholder return.27 In all there is no conclusive evidence how best to fund general practitioners and primary health care systems.26
As Hart28 points out, the basic economic question to be answered is: ‘What constitutes the unit of production’ in medical care? In the classic economic model ‘throughput’ would be the answer. This though contradicts our initial assumption that ‘health care’ is centred on the patient’s needs. Thus a more accurate answer would be that the production unit is the ‘value of the consultation’. Value is created by understanding the patient’s problem better and by the steps taken toward achieving healing.28
In such a model, costs are determined as a result of the joint decision between the doctor and the patient as to what is the best action in THIS patient’s context. This approach requires time, but time is the most expensive resource in a throughput model. On the contrary, in a patient-centred outcome model time is the most cost-saving resource, eliminating unnecessary and unwanted interventions. Thus quality and efficiency of care are usually best understood at the point of service delivery, and they should drive the resource utilization in consultations rather than by the ‘top down’ constrained understandings of financial managers.
There are many new developments such as new investigations and pharmaceuticals proclaiming to alleviate the burden of the modern epidemics of non-communicable chronic diseases. Many of these developments have not been properly evaluated18,29 in terms of their superiority compared to older well-established management strategies, and are often driven by profit-seeking industries rather than the real needs of patients.30
Lack of accountability (or quality of care)
The lack of measures that quantify what medicine, and general practice/family medicine in particular, actually does, has lead bureaucrats to invent artificial counting scales as surrogates to judge ‘health outcomes’. There is some evidence that much of what can be counted, and is now regarded as essential and sensible medical intervention, is actually causing substantial harm and leading to increased morbidity and mortality. True accountability requires evidence about clinical processes that have a positive impact on health. This is especially so for iatrogenic diseases generated by a re-definition of disease (e.g., hypertension, hyperlipidaemia and diabetes, by lowering the threshold values).18 It is also pertinent where lack of quality care may be unaccounted for because it is not measurable, such as in chronic illness care and time spent in patient-centred explanation and knowledge transfer.31
Health policies and an aging population
Our populations will become older very rapidly in the early 21st century, with the proportionately largest increases in the population occurring at the oldest ages, that is 85 and above.32,33 We are also becoming more obese and prone to lifestyle-linked chronic disease epidemics. The reason for concern in the growing number of the aged is related to health care outlays which link back to the other issues. Older people cost more in terms of time requirements as well as in economic outlay; indeed half of all health care cost is spent on the last 6 months of a patients’ life. Often the health system delivers heroic attempts to save a life in an acute care setting with little attention to the patient’s experience and needs.
General practice/family medicine – a confused entity
Gatekeeping
General practice/family medicine has been placed at the forefront of the health care system, being charged with gatekeeping. This can be interpreted as channelling patients into the most appropriate sector of the health care system, and/or limiting access and controlling cost within the health care system.
Integration in a fragmented world
Specialization of medicine according to disease and organ system entities has been spectacularly successful for a limited number of problems, resulting on the one hand in fragmented ‘health care’, and on the other it challenges the need for general practice/primary care services. Research within the tertiary medical environment has identified numerous risk factors associated with its disease spectrum. Risk factors are now seen as ‘diseases’ resulting not only in an explosion in the number of ‘non-disease’ entities34 but also leading to a ferocious effort of screening and treatment despite the fact that there is little evidence for improvement of clinically relevant outcomes in those affected.18 This preoccupation with ‘case finding’ undermines attention being paid to behavioral approaches to healthy living and the modification of high-risk attitudes and behaviors.
Role confusion
General practitioners/family physicians are consulted by people with any type of health problem,35 thus being at the interface of acute or disease-based care competing with the medical specialties and hospitals, and the chronic or illness-based care provided by a wide variety of agencies. As such their work is based on the five pillars of primary care – accessibility, comprehensiveness, coordination, continuity and accountability.36
However, under existing and new models of ‘managed care’ general practitioners’/family physicians’ tasks are challenging: dealing with expectations of cure, balancing personal care of an individual with best practice technical guidelines, and increasingly, to ration expensive health services.27,37 The general practitioner/family physician, at the bottom of the medical hierarchy, is being asked to be most responsive to ‘client demand’, and is increasingly asked to conform to ‘evidence’ and ‘protocols’ still largely dominated by specialist biomedical models.7,18,38,39
Conclusions
Health in the current climate is narrowly defined through economic and health service considerations, rather than the experience of the patient. Factors perpetuating this approach are linked through the dominance of economic concerns and tertiary level medicine and the medical education framework. This model is unsustainable – new medical developments, often implemented uncritically, exacerbate cost pressures and typically drain resources from other social portfolios. The general practitioner/family physician is squeezed within this system, having difficulties to operate effectively in response to unrealistic demands and loss of role definition.
A new vision and conceptual framework based on complex adaptive systems and the somato-psycho-socio-semiotic paradigm is required to address these issues on a real basis. Considerable self-organizing as a bottom-up dynamic must be generated through interactive bonding among key individuals who are stakeholders at each layer of the primary care system, but particularly at the level of care delivery.
In spite of economic and the wide range of other diverse challenges, general practice/family medicine must promote a ‘change vision’ and strategy to integrate and focus on front-line providers and meeting patients’ individual needs at the point of care, despite economic and tertiary care disease model drivers. General practice/family medicine is ultimately accountable to the patient, the community and the population to improve their health experiences with a realignment to a broader vision of health care.
References
1 Popper K. Conjectures and Refutations: the Growth of Scientific Knowledge. London: Routledge and Kegan Paul, 1972.
2 Senate Community Affairs References Committee. First report – Public hospital funding and options for reform. Canberra. Available at: http://www.aph.gov.au/senate/committee/clac_ctte/completed_inquiries/1999–02/phealth_first/report/report.pdf 2000.
3 Rosenberg C. The Tyranny of Diagnosis. Specific Entities and Individual Experience. Milbank Q 2002; 80: 237–60.
4 Glouberman S, Zimmerman B. Complicated and Complex Systems: What Would Successful Reform of Medicare Look Like?: Discussion Paper No. 8. Commission on the Future of Health Care in Canada, Otawa, 2002.
5 Pauli H, White K, McWhinney I. Medical Education, Research, and Scientific Thinking in the 21st Century (Part one of three). Educ Health 2000; 13: 15–25.
6 Fugelli P. Trust. Gen Pract 2001; 51: 575–9.
7 Sturmberg JP. The Foundations of Primary Care. Daring to be Different. London: Radcliffe Publishing, 2007.
8 Capra F. The Web of Life. London: HarperCollins Publishers 1996.
9 McDaniel Rj. Strategic Leadership. A View from Quantum and Chaos Theories. Health Care Manage Rev 1997; 22: 21–37.
10 Beckman H, Frankel R. The Effect of Physician Behavior on the Collection of Data. Ann Intern Med 1984; 101: 692–6.
11 Martin C, Banwell C, Broom D, Nisa M. Consultation length and chronic illness care in general practice: a qualitative study. Med J Aust 1999; 171: 77–81.
12 Gottlieb E. The great x-ray mystery. J Pract Orthodon 1969; 3: 486–93.
13 Speckens A, van Hemert A, Spinhoven P, Hawton K, Bolk J, Rooijmans H. Cognitive behavioural therapy for medically unexplained physical symptoms: a randomised controlled trial. Br Med J 1995; 311: 1328–32.
14 Kiecolt-Glaser J, McGuire L, Robles T, Glaser R. Psychoneuroimmunology. Psychological Influences on Immune Function and Health. J Consult Clin Psychol 2002; 70: 537–47.
15 Cox K. Who’s My Doctor Today? Educ Health 2002; 15: 370–5.
16 White K, Williams F, Greenberg B. The Ecology of Medical Care. N Engl J Med 1961; 265: 885–92.
17 Mayou R, Sharpe M. Treating medically unexplained physical symptoms. Br Med J 1997; 315: 561–2.
18 Fisher E, Welch H. Avoiding the Unintended Consequences of Growth in Medical Care. Hwo Might More Be Worse? J Am Med Assoc 1999; 281: 446–53.
19 Nielsen M, Thomsen J, Primdahl S, Dyreborg U, Andersen J. Breast cancer and atypia among young and middle-aged women: a study of 110 medicolegal autopsies. Br J Cancer 1987; 56: 814–9.
20 Harach H, Franssila K, Wasenius V. Occult papillary carcinoma of the thyroid. A ‘normal’ finding in Finland. A systematic autopsy study. Cancer 1985; 56: 531–8.
21 Montie J, Wood DJ, Pontes J, Boyett J, Levin H. Adenocarcinoma of the prostate in cystoprostatectomy specimens removed for bladder cancer. Cancer 1989; 63: 381–5.
22 Whitehead M. Diffusion of Ideas on Social Inequalities in Health: a European Perspective. Milbank Q 1998; 76: 469–92.
23 Subramanian S, Belli P, Kawachi I. Macroeconomic Determinants of Health. Annu Rev Public Health 2002; 23: 287–302.
24 Wilkinson R. Unhealthy Societies: the Afflictions of Inequality. London: Routledge 1996.
25 Cohen S. Psychosocial models of the role of social support in the etiology of physical disease. Health Psychol 1988; 53: 1066–74.
26 Gosden T, Forland F, Kristiansen I, et al. Capitation, salary, fee-for-service and mixed systems of payment: effects on the behaviour of primary care physicians. The Cochrane Library 2004 (Issue 4).
27 Bodenheimer T. The HMO Backlash – Righteous or Reactionary? N Engl J M 1996; 335: 1601–4.
28 Hart J. What evidence do we need for evidence based medicine? J Epidemiol Community Health 1997; 51: 623–9.
29 Cochrane A. Effectiveness and efficiency. Random reflections on health services. London: The Nuffield Provincial Hospitals Trust, 1972.
30 Moynihan R, Heath I, Henry D. Selling sickness: the pharmaceutical industry and disease mongering. Br Med J 2002; 324: 886–91.
31 Martin C, Attewell R, Nisa M. Chronic care in adulthood and old age: physical and psychosocial management in general practice encounters. Aust J Prim Health Care 2000; 6: 57–67.
32 Hogan S, Hogan S. How Will the Ageing of the Population Affect Health Care Needs and Costs in the Foreseeable Future? Available at: http://collection.nlc-bnc.ca/100/200/301/pco-bcp/commissions-ef/future_health_care-ef/discussion_paper-e/no25/25_e.pdf Commission of the Future of Healthcare in Canada, 2002.
33 Bloor K, Maynard A. Planning human resources in health care: Towards an economic approach. An international comparative review. Canadian Health Services Research Foundation. (National informants: Australia: Professor Jane Hall, Centre for Health Economics Research and Evaluation; France: Dr Phillippe Ulmann, Conservatoire National des Arts et Metiers de Paris; Germany: Dr Oliver Farhauer, Technical University, Berlin and European Centre for Comparative Government and Public Policy; Sweden: Professor Bjõrn Lindgren, Lund University.) Ottawa: Canadian Health Services Research Foundation, 2003. Available on the web: http://www.chsrf.ca/final_research/commissioned_research/programs/pdf/bloor_report.pdf
34 Meador C. The Art and Science of Nondisease. N Engl J Med 1965; 272: 92–5.
35 McWhinney I. Family Medicine in Perspective. N Engl J Med 1975; 293: 176–81.
36 Starfield B. Primary Care. Balancing Health Needs, Services, and Technology. Revised edn. Oxford: Oxford University Press, 1998.
37 Schlesinger M, Mechanic D. Challenges for managed competition from chronic illness. Health Affairs (Millwood) 1993, 2000; 12: 123–37.
38 Primary Care and Health: 21st Century Challenges to Quality. The General Practice Evaluation Program. The 2000 General Practice Evaluation Program Conference Proceedings, September 2000, Adelaide, Australia. Adelaide: National Information Service, Department of General Practice, Flinders University, 2000.
39 Lauritzen T, Mainz J, Lassen J. From science to everyday clinical practice. Need for systematic evaluation of research findings. Scand J Prim Health Care 1999; 17: 6–10.
Figure 1 - Disease-focused health care focuses on costs, patient-focused health care focuses on patient-relevant health outcomes
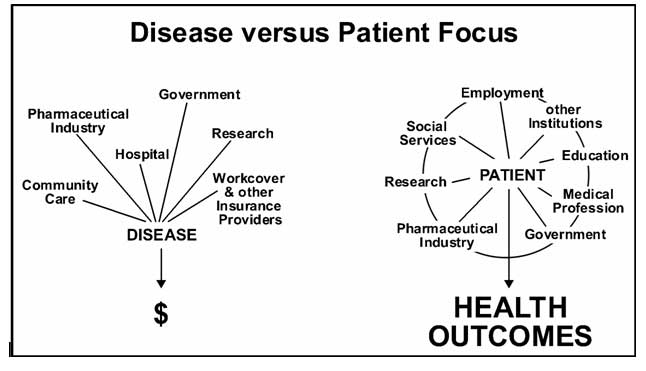
Figure 2 - The Health Care Vortex – all activity within the health system ultimately effects cellular health
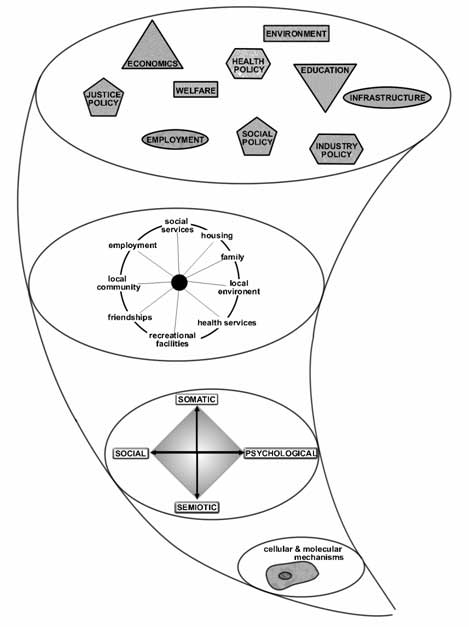
Figure 3 - Perpetuating the disease model – Dominance over the Disease over the Illness Model
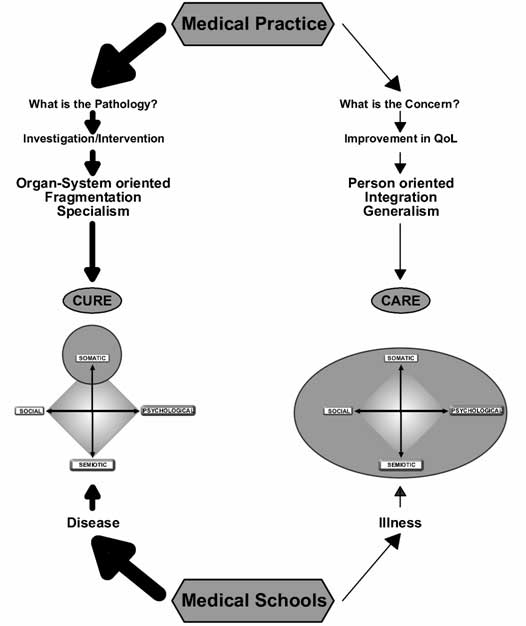
Figure 4 - The main forces that shape the health care system – Pressures on the Health System

^top